

Surest, a UnitedHealthcare company, administers a health plan without a deductible or coinsurance. Members have access to the Optum and UnitedHealthcare network and can check costs and care options in advance.
To help you work with Surest plan members and claims, please visit surest.com/providers.
While Surest plans leverage the Optum and UnitedHealthcare networks, these members must present their Surest member ID card.
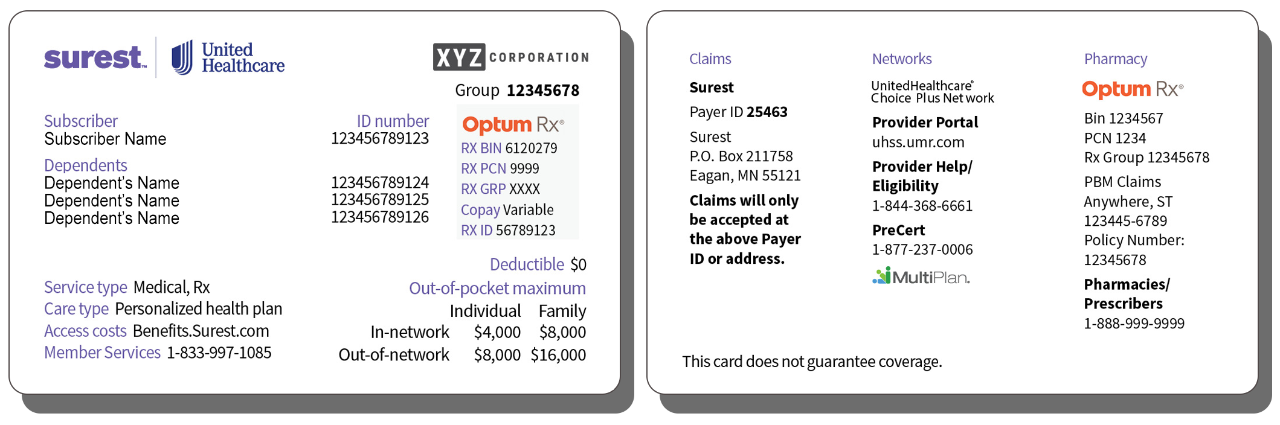
Sample member ID card for illustration purposes only; actual information varies depending on payer, plan and other requirements.
Please include the subscriber ID and rendering address on the claim to help us confirm the copay/member price.
To check eligibility and benefits, visit the UnitedHealthcare Shared Services (UHSS) Provider Portal or call UHSS Provider Services at 844–368–6661. You’ll need to provide the subscriber ID if you’re requesting information about a dependent.
What do I need to know about member copays and my reimbursements?
To help ensure pricing reflects the best and most recent data, member copays/prices are updated annually. Accordingly, you always need to check the current member copay/price before collecting payment for a service. Although a service's member copay/price may change, your contracted rate for the service doesn’t.
Note: Member copays/prices for a service can vary by facility and/or health care professional.
What’s the process for prior authorization?
The prior authorization/notification requirements in the UnitedHealthcare Administrative Guide apply to Surest plans. Please call 1-877-237-0006 for all precertification needs or questions.
We should ask if there is an Optum guide that we may be missing out on.
How can I check the status of a claim?
To check claim status, visit the UHSS Provider Portal or call UHSS Provider Services at 844-368-6661.
How can I file a claim reconsideration?
Please send claim reconsiderations to:
Mail: UHSS, Attn: Claims, P.O. Box 30783, Salt Lake City, UT 84130
Fax: 866-427-7703
If applicable, please send the claim to the attention of the representative with whom you spoke.
How can I file a clinical appeal?
Note that clinical appeals are only for services that received a medical necessity review and weren’t determined to be medically necessary.
Please send clinical appeals to:
Mail: UHC Appeals — UHSS, P.O. Box 400046, San Antonio, TX 78229
Phone: 800-808-4424, ext. 15227
Fax: 888-615-6584
Remember to provide all supporting materials in your appeal, including member-specific treatment plans and clinical records.